What is a Cataract?
Cataract BrochureA cataract is a clouding of the lens in the eye that affects vision. Most cataracts are related to aging. Cataracts are very common in older people. By age 60, more than half of all Indian patients have either developed a cataract or have had cataract surgery. A cataract can occur in one or both eyes. It cannot spread from one eye to the other.
What is the lens?
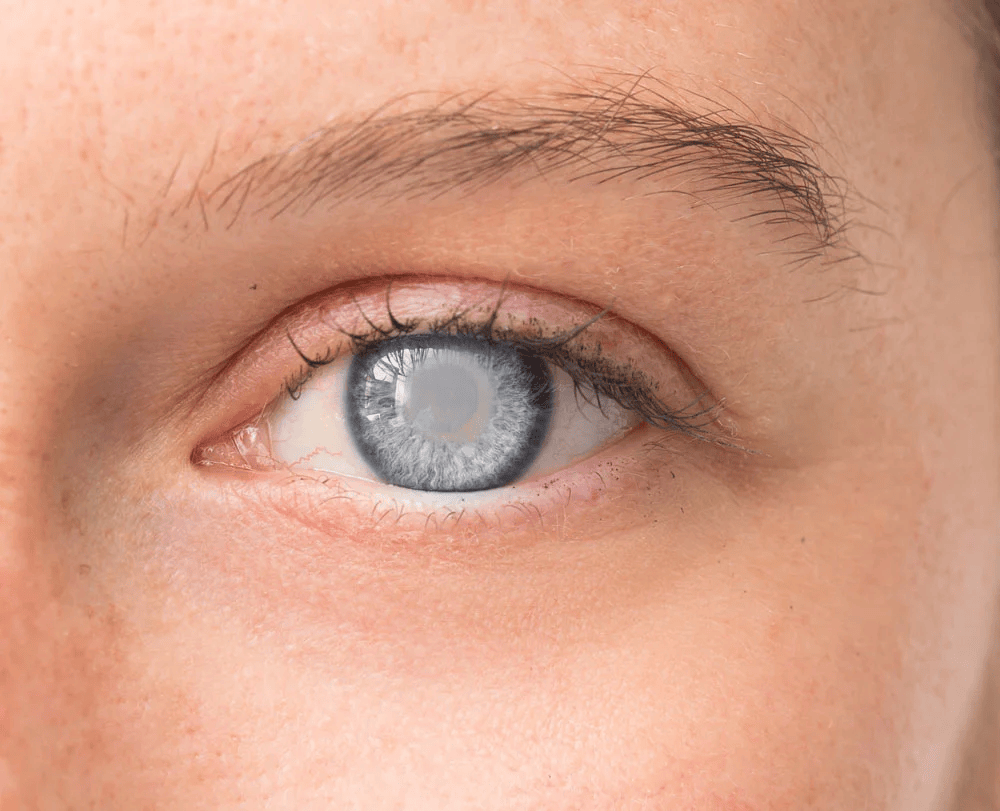
The lens is a clear part of the eye that helps to focus light, or an image, on the retina. The retina is the light- sensitive tissue at the back of the eye. In a normal eye, light passes through the transparent lens to the retina. Once it reaches the retina, light is changed into electrical signals that are sent via the optic nerve the brain. The lens must be clear for the retina to receive a sharp image. If the lens is cloudy from a cataract, the image you see will be blurred.
What are the symptoms of a cataract?
The most common symptoms of a cataract are:
• Cloudy or blurry vision, decreased reading vision.
• Colors seem faded.
• Glare, Headlights, lamps, or sunlight may appear too bright.
• A halo may appear around lights.
• Poor night vision.
• Double vision or multiple images in one eye. (This symptom may clear as the cataract gets larger).
• Frequent prescription changes in your eyeglasses or contact lenses.
THE MOST FREQUENT SYMTOMS OF CATARACT ARE
- Diminished vision and glare – In the early stages only distance vision may suffer or the oncoming headlights at night can cause unbearable glare.
- As it progresses reading vision can suffer along with a change in spectacle number. People forced to wear reading glasses will find they can go without them. This is called Second Sight and indicates the formation of a Cataract.
- Sometimes because of swelling of the cataract, the pressure in the eye goes up and the patient complains of mild heaviness or headache.
CATARACT CAN DEVELOP AT ANY AGE
- Newborns can have cataract due to infection in the womb commonly due to rubella.
- Young children can develop cataract due to metabolic imbalances and infections—for example, inability to digest milk is sometimes associated with cataract.
- Any blow to the eye in play and even severe malnutrition can lead to cataract in childhood.
- The use of steroid-containing skin creams for months, putting steroid anti-allergy eye drops for a long period of time and exposure to sunlight can cause cataracts in the 20–40 year age group.
- Cataract is seen in glassblowers and in foundry workers due to infrared rays and so it’s advisable to have protective dark spectacles in these professions.
- Diabetes, other eye diseases, Glaucoma and even any eye surgery or retinal detachment lead to Cataract. Anytime there is an internal eye disease, a Cataract is a likely result!
- In old age the most common type of Cataract called Senile Cataract is seen. This is because the proteins in the human lens congeal and coagulate like egg white in a frying pan leading to a whiteness.
- Finally, exposure to radiation—for example, nuclear power plant technicians and people undergoing radiotherapy for cancer of the head and neck—are likely to develop Cataract.
CATARACT PREVENTION
- Avoid blows to the eye in sports like squash and badminton by wearing protective spectacles (mandatory in the west).
- Make sure your diet has the necessary vitamins and minerals.
- Follow your gynecologist’s advice at the time of conception and delivery and do appropriate blood tests as recommended by them.
- Sunlight exposure is a prominent cause, so do not venture in the sun without sufficiently dark sunglasses.
- If you work in a steel mill or any area where a lot of red heat is present, make sure you wear eye protection.
- Do not put on steroid creams indiscriminately or use eye drops long after the doctor has stopped prescribing them.
ARE THERE OTHER TYPES OF CATARACT?
- Yes. Although most cataracts are related to aging, there are other types of cataracts.
- Secondary cataract:Cataracts can form after surgery for other eye problems, such as glaucoma. Cataracts also can develop in people who have other health problems, such as diabetes. Cataracts are sometimes linked to steroid use.
- Traumatic cataract:Cataracts can develop after an eye injury, sometimes years later.
- Congenital cataract:Some babies are born with cataracts or develop them in childhood, often in both eyes. These cataracts may be so small that they do not affect vision. If they do, the lenses may need to be removed.
- Radiation cataract:Cataracts can develop after exposure to some types of radiation.

How is a cataract detected and fully evaluated?
Cataract is detected through a comprehensive eye exam that includes:
• Visual Acuity Test: This eye chart test measures how well you see at various distances and
prescribes the correct spectacles after checking the details with an Auto Refractor.
• Slit Lamp Bio Microscope Evaluation: Using a high-powered microscope the eye is examined in
detail and the cataract is evaluated, with its density and any complicating circumstances.
• Retinal Examination: Drops are placed in your eyes to widen, or dilate, the pupils. Subsequently with an
indirect ophthalmoscope which enlarges the retinal image and your retina and optic nerves are assessed
for signs of damage and other eye problems.
- Tonometry: The doctor will test your eye pressure with an Air Puff Pneumo Tonometer. Alternatively, an instrument that measures the pressure called an Applanation Tonometer can be placed on that the clear cornea after applying numbing drops.
- Contrast Sensitivity Testing: Utilizing special charts with a grating system the doctor can tell how far the cataract has developed and even the speed of development and when he would expect the cataract would be ready for removal.
- Ultrasound B Scan Sonography: If the cataract is very dense it is not possible to know what is the status of the retina. In this circumstance, the doctor will use a B Scan device that uses ultrasound to image the retina. Unfortunately, it can only tell if the retina is in place, but not if it functions or if there is any pathology like macular degeneration.
- Specular Microscopy: Finally the cells on the inner side of the cornea are assessed to be sure that they would not be affected by the energy used to remove the cataract. If they are weak, then a special protective viscous liquid is used during cataract surgery.
- A Scan Sonography: This is done to evaluate the exact power of the implant which, when placed in your eye will bring the resultant power to a range of+/- 1.5D.
A common question often by patients is why even with the most sophisticated biometry units, still the power of the eye, following surgery does not go down to zero. The reason is simple. The implant is fitted in the eye, behind the pupil, into soft tissue. A difference of 1 mm in the accuracy of the fitting leaves a result of almost +/- 3.00. Thus the accuracy of a third of a millimeter, equivalent to a +/-1.00 D is the maximum one can expect. In addition, some astigmatism is expected as the healing process of an eye is an unknown factor and cannot be exactly predicted. Hence little astigmatism which normally decreases with time is also expected.
ARE THERE DIFFERENT TYPES OF CATARACT SURGERY?
INTRACAPSULAR CATARACT SURGERY
EXTRACAPSULAR SURGERY
PHACOEMULSIFICATION, OR PHACO
SUCCESS RATES
MICROPHACO
INFINITI AQUALASE CATARACT SURGERY
INFINITI OZIL CATARACT SURGERY
WHY INFINITI IS THE MOST ADVANCED, THE LATEST INSTRUMENT FOR CATARACT SURGERY?
WHAT DOES IT DO?
THE INFINITI CATARACT REMOVAL SYSTEM
- A revolutionary new surgical device for safer, cataract surgery, it puts unprecedented precision, perfection and performance to and virtual total safety in cataract surgery.
- This system utilizes a revolutionary new device termed the Aqualaser Liquifactor. AquaLase® Liquefaction Device is part of the Infiniti™ Vision System and is the world’s first tri-modal cataract removal surgical instrument.
- Utilizes the new OZIL dual ultrasound technique to remove lenses very fast especially hard cataracts.
- Advanced ultrasound phacoemulsification alone with, the ability to use micropulses or hyperpulses.
- The combination of ultrasound and oscillation energy is provided by the NeoSonix® headpiece.
- The New AquaLase® liquefaction device, utilizes a micro fluid, high energy pulses, of only five milliseconds, which gently and with great safety, dissolve the cataract.
- New Ozil technology, is ideal for hard cataracts and for sensitive corneas.
The Infiniti system uses a sensitive intelligent high-end computer interface with digital control, and pressure sensors monitoring in real-time, enhancing safety.
The greatest advantage of the new machine, of course with the AquaLaser liquifactor device is that it dramatically reduces the potential for complication thanks to its innovative soft, fluid pulses. This new advancement in lens removal technology is a quantum leap forward and significantly improves results following cataract surgery.
The new OZil system utilizes dual ultrasound movement both longitudinal and oscillatory to make cataract removal especially hard cataracts now very safe with simultaneous safety for the very delicate endothelial cells at the back of the cornea.

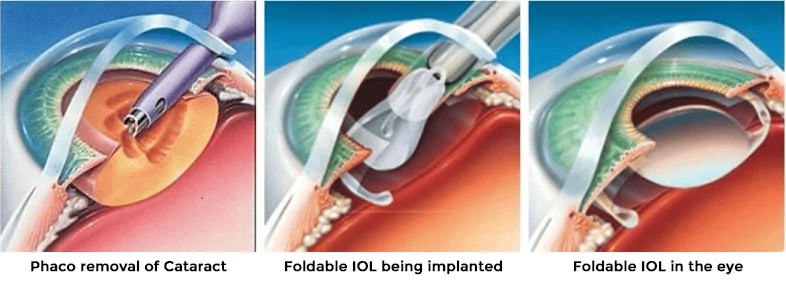
WHAT HAPPENS DURING SURGERY?
At the operating facility, drops will be put into your eye to dilate the pupil. The area around your eye will be washed and cleansed with an antibiotic solution.
The operation, Phaco or AquaLase usually lasts about 5‑8 minutes and is virtually painless. Many people choose to stay awake during surgery. Others may opt to be put to sleep for a short time. If you are awake, you will have anesthetic eye drops to numb the nerves in and around your eye. You will be asked to look into the light and to keep your eyes fixed on the light for 6 minutes. During the procedure, you will feel a bit tight and will feel water running out of the eye but you will have no pain whatsoever.
After the operation, a protective sterile clean plastic shield or glasses will be placed over your eye. You will rest for a while. Your medical team will watch for any problems, such as discomfort. Most people who have cataract surgery can go home an hour following surgery. You will need someone to accompany you or drive you home.
WHAT HAPPENS AFTER SURGERY?
- Itching and mild discomforts are normal after cataract surgery. Some poking and a fluid discharge especially on the first day are also common. Your eye may be sensitive to light and touch. You may see objects colored on the first day.
- From the next day the eye becomes quiet, watering becomes very less, though it will still be a bit moist, and poking gradually goes away.
- No water must be applied inside the eye for 4 days though you can have a head bath with your eyes closed from the day onwards.
- When you are home, try not to bend from the waist to pick up objects on the floor. Do not lift any heavy objects. You can walk, climb stairs, and cook. But for 10 days do light household chores, with no heavy lifting.
- In most cases, healing will be complete within four weeks. Your doctor will schedule exams to check on your progress.
- For three months following the surgery, your doctor will ask you to use eye drops to help heal and decrease the risk of infection. You will need to wear an eye shield or eyeglasses to help protect your eye. Avoid rubbing or pressing on your eye.
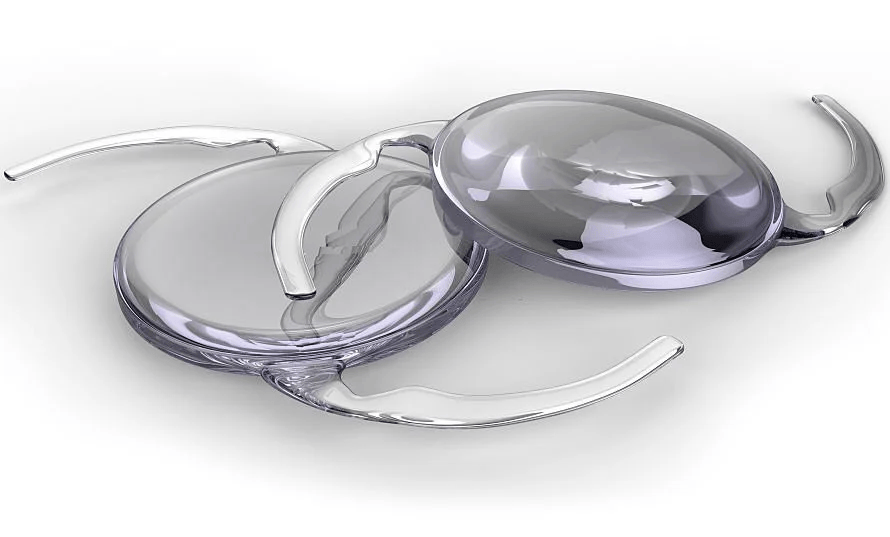
WHAT TYPE OF IOL SHOULD I IMPLANT IN THE EYE?
Intraocular lenses, commonly called IOLs, may be one of the most important ophthalmic developments in the past 30 years. These tiny prescription lenses are placed inside the eye during cataract extraction, replacing the eye’s natural lens (called a cataract when it becomes clouded). Prior to the development of IOLs, cataract patients were forced to wear thick “soda-water bottle” glasses or contact lenses after the surgery. They were essentially blind without their glasses.
Today, patients receiving IOLs often enjoy the best vision of their lives. Thanks to sophisticated formulas used to calculate the corrective prescription power of the lens, the IOL not only replaces the need for thick glasses but can also correct the eye’s existing refractive error.
There are two basic types of IOLs: foldable and hard. Foldable lenses are made of silicone or acrylic and can be rolled up and placed inside a tiny tube. The tube is inserted through a very small incision – less than 2.5 mm in length. Once inside the eye, the IOL gently unfolds. Hard plastic lenses are appropriate in certain circumstances determined by the surgeon. Since they cannot be folded, they are placed through a slightly larger incision.
The first intraocular implant in regular practice was implanted in Bombay by Dr. Keiki R. Mehta in 1972. He is also the developer of the world’s first soft intraocular implant in 1978. He has recently developed the world’s first actively Clamshell accommodative IOLs for which trials are proceeding.

SHOULD I IMPLANT A MULTIFOCAL IMPLANT IN MY EYE? WHAT ARE THE ADVANTAGES AND DISADVANTAGES?

The human lens accommodates, i.e. see far and near, by changing the shape of the human lens. When it becomes thicker the power increases for near and when it thins out, for distance. However, a plastic implant cannot do so. In an effort to return a modicum of accommodation to the patient, Multifocal lenses have been devised.
There are two types of Multifocal implants. Fixed and Variable. Fixed Multifocal implants use different rings of power, alternative for distance and near on the same implant. Thus simultaneous vision is available for both distance and near. However, the side effect of these implants is that glare around a light, especially in dark places and at night is inevitable. It also means that driving at night may sometimes be difficult as haloes will be seen around the lights.
The second problem is that part of the distance vision is used for near which leads to a fall in contrast. Thus though the vision in a bright light situation is perfect, at dusk or in poor light situations vision will be a little ‘soft’. If you do not drive at night and are not overtly dependent on reading glasses or need to read the whole day then Multifocal may be your answer to have reasonably good vision for both distance and near.
Multifocals are ideal for business people dealing with customers across the table needing eye contact. They are excellent for housewives. They are easily fitted in children who have cataracts, as a child adapts to multifocal implants very fast and is not bothered by light reflections.
Multifocal Implants BrochureWHAT ARE THE LATEST ‘VARIABLE FOCAL’ MULTIFOCAL IMPLANTS?
These lenses ( called the Crysta lens) are actively mobile implants that move forwards for near and settle back for near. Most important of all they give no glare or flare or rings around the light which was the bane of the “fixed” multifocal implants. Though they are costly (cost around 3 times more than regular multifocal lenses ) they give excellent vision for distance and intermediate and reasonably good vision for near, and they do it with no optical disturbances.
However, for reading the very fine print you may still need to use glasses. Since it is no glare and flare are seen in these lenses, one can drive at night reasonably comfortably. Great value though a bit costly.
WHEN WILL MY VISION BE NORMAL AGAIN AFTER CATARACT SURGERY?
You can return quickly to many everyday activities, but your vision may be blurry. The healing eye needs time to adjust so that it can focus properly with the other eye, especially if the other eye has a cataract. Ask your doctor when you can resume driving. If you received an IOL, you may notice that the colors are very bright. Within a few months after receiving an IOL, you will become used to improved color vision. Also, when your eye heals, you may need new glasses or contact lenses.
WHAT ARE THE RISKS OF CATARACT SURGERY?
As with any surgery, cataract surgery poses risks, such as infection and bleeding. Before cataract surgery, your doctor may ask you to temporarily stop taking certain medications that increase the risk of bleeding during surgery. After surgery, you must keep your eye clean, wash your hands before touching your eye, and use the prescribed medications to help minimize the risk of infection. Serious infection can result in loss of vision.
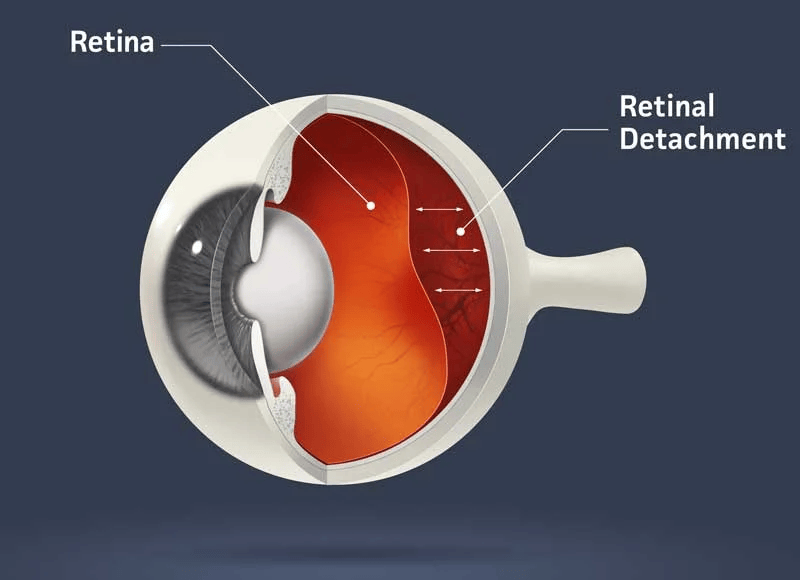
Cataract surgery may slightly increase your risk of retinal detachment. Other eye disorders, such as high myopia (nearsightedness), can further increase your risk of retinal detachment after cataract surgery. One sign of a retinal detachment is a sudden increase in flashes or floaters. Floaters are little “cobwebs” or specks that seem to float about in your field of vision. If you notice a sudden increase in floaters or flashes, see the doctor immediately.
WHAT IS AN AFTER-CATARACT?
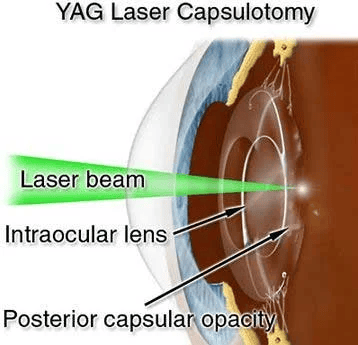
During cataract surgery, a clear capsule surrounding the cataract is left in place to support the lens implant. In some cases, this capsule may turn cloudy months or years after surgery creating, what is called, an after-cataract. An after-cataract can develop months or years later. Unlike a cataract, an after-cataract is treated with a laser. In a technique called YAG laser capsulotomy, your doctor uses a laser beam to make a tiny hole in the lens to let light pass through. This is a painless outpatient procedure.
LASIK AFTER CATARACT REMOVAL
“LASIK” is an acronym for Laser In-situ Keratomileusis, which simply means, “to shape the cornea from within using a laser.” Its “cool” or non-thermal light beam corrects vision by reshaping the cornea (outer window of the eye) so that light rays focus more precisely on the retina, thereby eliminating or reducing refractive errors and the need for glasses or contacts.
Since the LASIK procedure is performed on the surface of the cornea, (see diagram) and with cataract surgery, the lens implant is placed through the pupil, behind the colored iris, neither area is negatively affected by the other surgery.
If you had cataract surgery, say 5 years ago, and you require LASIK to improve your myopia (nearsightedness), hyperopia (farsightedness) or astigmatism, the LASIK procedure would reshape the front of your cornea and would not adversely affect the positive results achieved with your prior cataract removal and lens implant surgery.
Multifocal patients may need to have their cornea’s polished to enhance the quality of vision using an excimer laser. Here no flap is lifted(like in Lasik) but the laser is only applied to the surface ( called surface ablation) A few days of discomfort and the vision becomes sharp.
What if I have other eye conditions and need cataract surgery?
Many people who need cataract surgery also have other eye conditions, such as age‑related macular degeneration or glaucoma. Having another eye problem is only important as far as it affects the final visual outcome following the cataract surgery. For example, if you have central retinal degeneration, the only improvement likely following a cataract is to enhance the side vision and improve clarity—but the number of lines in the chart you can see will remain the same. It differs from patient to patient.
Catalys FemtoSecond Laser Brochure